The Architecture of Access: Why Wait Times Are a Design Flaw, Not a Resource Deficit
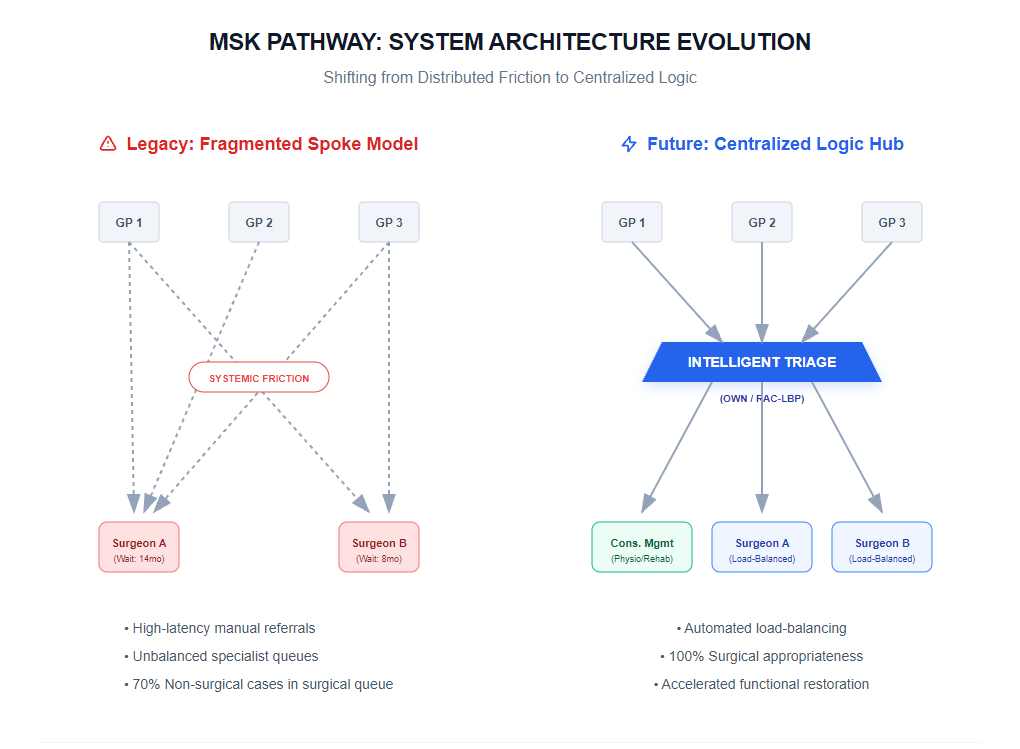
Shifting the MSK Narrative from "More Surgeons" to "Smarter Logic" through Centralized Intake and Triage.


Addressing Ontario’s MSK backlog requires more than additional OR hours; it demands a fundamental redesign of the patient pathway. By treating wait times as systemic friction, we can implement architectural solutions like OWN and RAC-LBP to restore function at scale.
I. The Problem: Systemic Friction in the Pathway
In the current Ontario musculoskeletal (MSK) landscape, wait times are frequently misdiagnosed as a "lack of surgeons" or "insufficient funding." This is a fundamental misunderstanding of the problem. What we are actually witnessing is systemic friction.
The traditional referral model is fragmented, siloed, and high-latency. A patient enters a "black hole" of administrative drag where data is non-transferable and triage is inconsistent. When a patient waits 12 months for a consultation only to be told they are not a surgical candidate, that is not a resource failure—it is a catastrophic failure of system architecture. We are burning the most expensive resource in the system (surgical expertise) on diagnostic filtering that should have occurred months earlier.
II. The Observation: Clinical Logic at the OR-to-Cloud Intersection
As a Surgeon-CTO, I view the patient journey as a data pipeline. In any high-performance architecture, throughput is limited by the quality of the intake logic. Currently, our "logic" is manual and distributed across thousands of disparate primary care offices, leading to:
- Information Asymmetry: Surgeons receiving incomplete data, necessitating repeat imaging.
- Mismatched Capacity: Surgeons with open slots while nearby colleagues are drowning in backlogs.
- Triage Inefficiency: Up to 70% of MSK referrals do not require surgery, yet they occupy the same high-stakes intake channel as those who do.
The clinical reality is that "Functional Restoration" begins the moment a patient seeks help, not when they reach the operating table. If the system cannot route a patient to the right level of care—be it conservative management, specialized physiotherapy, or surgery—on the first attempt, the architecture is broken.
III. The Scalable Action: Building the Infrastructure of Recovery
To solve for wait times, we must stop asking for more "hardware" (surgeons and hospitals) and start optimizing the "operating system." We achieve this through Central Intake and Triage Logic, exemplified by models like the Ontario Wellness Network (OWN) and Rapid Access Clinics (RAC-LBP).
This is the Force Multiplier approach:
- Centralized Intake: Move from a "push" model (GP to individual surgeon) to a "pull" model (GP to a regional competency hub). This levels the load across the entire system.
- Advanced Practice Triage: Utilize highly trained physiotherapists as the "System Architects" of the front end. By filtering non-surgical cases early, we ensure surgeons only see patients ready for intervention.
- Data-Driven Matching: Implement algorithmic routing based on urgency, geography, and sub-specialty expertise to eliminate the "hidden cracks" where patients traditionally get lost.
The Metric of Success:
By implementing this architectural shift, we don't just reduce a number on a spreadsheet; we accelerate the path to Functional Restoration. We transform a legacy, friction-heavy process into a streamlined Infrastructure of Recovery that can scale regionally.

_web.png)