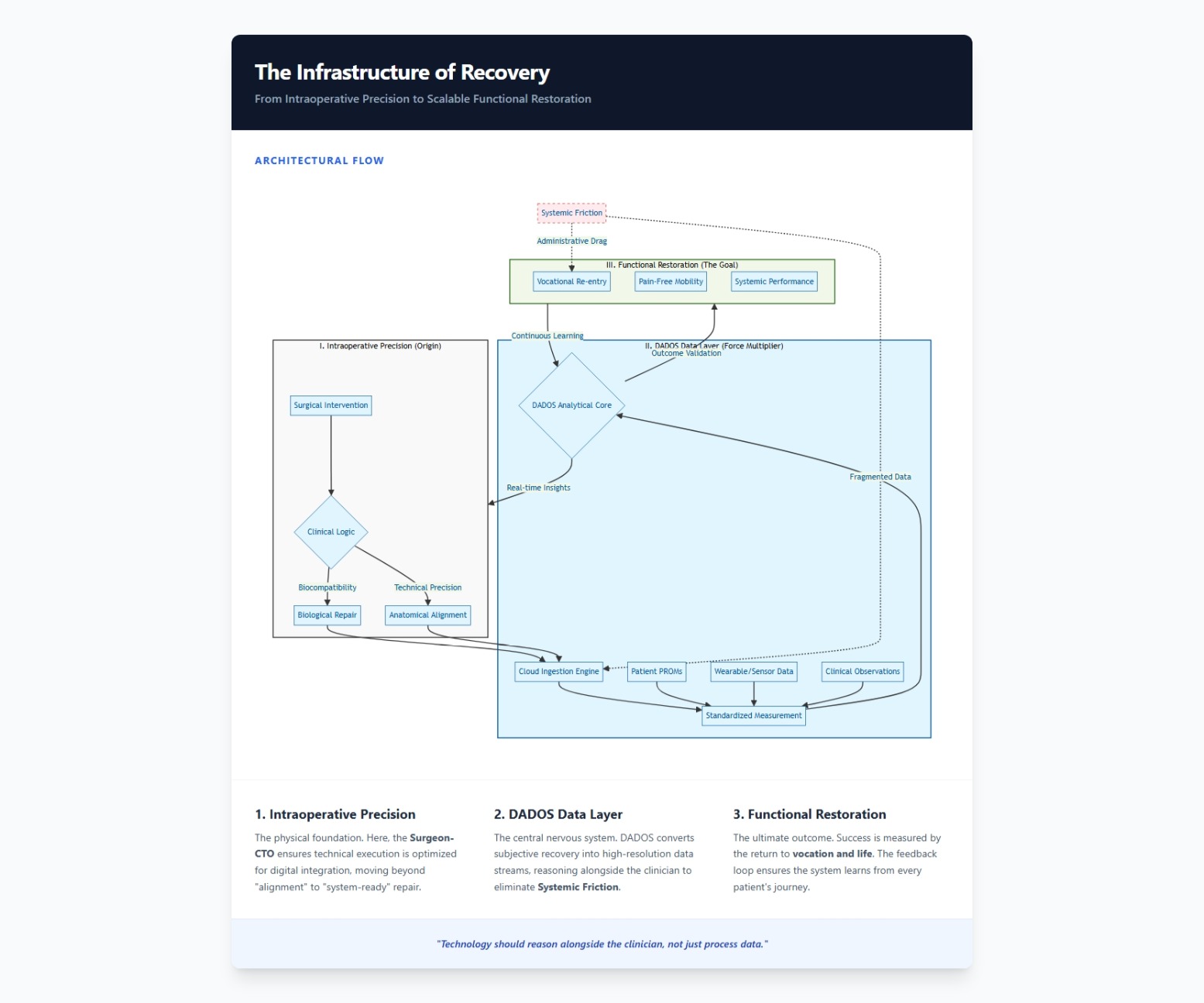
Beyond Biological Repair: The Infrastructure of Functional Restoration
Shifting the surgical mandate from anatomical correction to measurable human performance through data-driven clinical logic.


I. The Problem: The Friction of Anatomical Success
In the traditional orthopaedic model, success is often defined by the "perfect" X-ray. We celebrate a well-aligned fracture, a centered prosthesis, or a stable ligamentous repair. However, this focus on biological repair creates a massive gap in healthcare delivery—a form of systemic friction where the surgeon is satisfied, but the patient remains functionally bankrupt.
The friction lies in the disconnect between technical execution and the patient’s lived reality. A patient doesn't seek a "technically sound total hip replacement"; they seek the ability to walk to their office, play with their children, or return to their vocation without the cognitive load of pain. When we measure success solely through the lens of the operating room, we ignore the administrative and clinical drag that occurs during the long, unmonitored tail of recovery.
Current biological solutions fail to scale because they are treated as isolated events rather than a continuous arc of Functional Restoration.
II. The Observation: Clinical Logic at the OR-to-Cloud Intersection
As a Surgeon-CTO, my observation is that we have historically lacked the Clinical Logic to bridge the gap between "repair" and "function." In the operating room, we are precise; in the post-operative monitoring phase, we are often blind. This is where technology must act as a Force Multiplier.
The primary hurdle is that "function" is subjective until it is quantified. If we cannot measure the patient’s return to their life with the same precision we use to measure a 2mm bone graft, we aren't practicing value-based care—we are practicing high-cost guesswork.
To move toward a true Infrastructure of Recovery, we must integrate the surgeon's clinical intuition with a robust data architecture. We need to transition from asking "How does the wound look?" to "How is the human performing?" This requires a system that reasons alongside the clinician, capturing the nuance of recovery in real-time.
III. The Scalable Action: Systemic DNA and the DADOS Framework
To scale the path to recovery, we must embed outcome measurement into the very Systemic DNA of the surgical process. This is the core philosophy behind DADOS (Data-Driven Outcomes System). We move from anatomical snapshots to a longitudinal stream of functional metrics.
The Strategy for Functional Restoration:
- Quantify the Vocation: Success must be indexed against the patient's return to work and life. If a surgeon "fixes" a shoulder but the patient cannot return to their trade, the system has failed.
- The DADOS Multiplier: Use standardized outcome measurement to transform individual surgical successes into institutional benchmarks. We use this data to identify which technical interventions yield the highest functional ROI.
- Infrastructure of Recovery: By digitizing the recovery arc, we remove the friction of siloed data. The cloud becomes an extension of the clinic, allowing for proactive intervention before functional plateaus become permanent disabilities.
Impact Metrics for Success:
- Functional Velocity: The time elapsed from intervention to vocational return.
- Value-Based Precision: The correlation between surgical cost and measurable pain reduction.
- Systemic Scalability: The ability to replicate high-functioning outcomes across a global patient population.
We are no longer just "fixing anatomy." We are building the technical and clinical architecture required to restore human potential at scale.

_web.png)